Visualizing the Benefits of High-Risk Care Coordination in the Medicaid Population
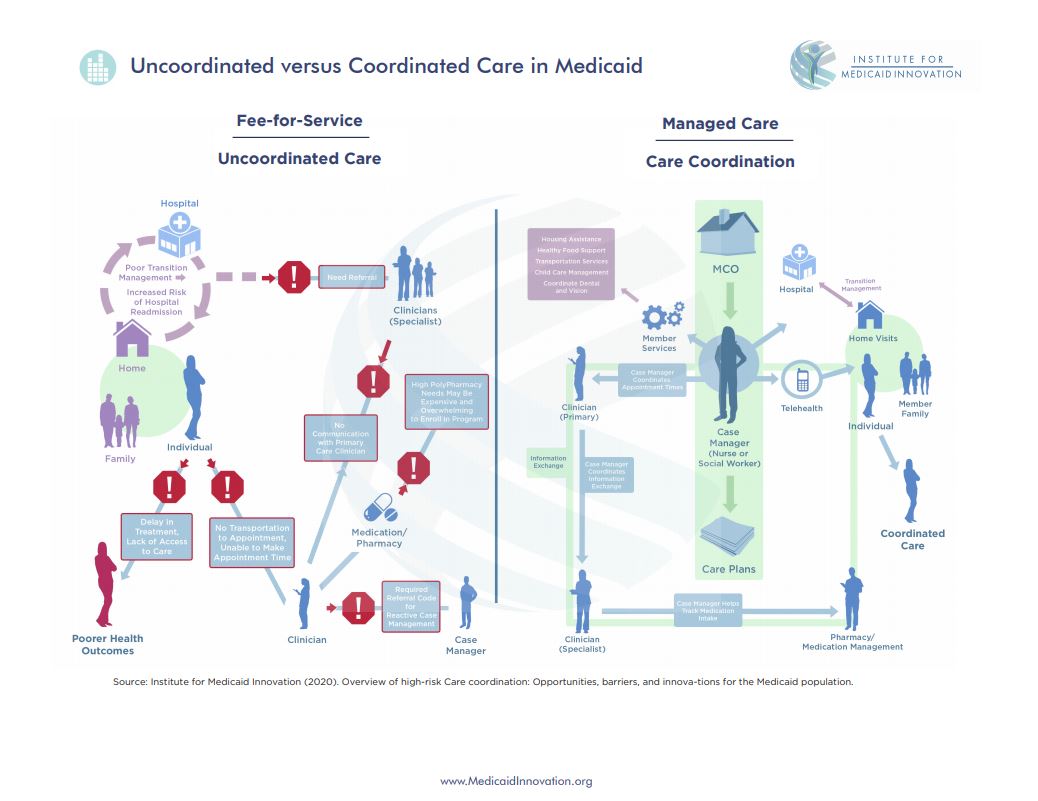
The recently released report by the Institute for Medicaid Innovation, High-Risk Care Coordination: Opportunities, Barriers, and Innovative Initiatives in Medicaid, includes an overview of the benefits of high-risk care coordination (HRCC) in the Medicaid population, highlights innovative case studies from Medicaid health plans, and describes the key components of HRCC programs, common payment mechanisms, and potential challenges to implementation. The report also features a comprehensive infographic which depicts the differences between uncoordinated and coordinated care in Medicaid.
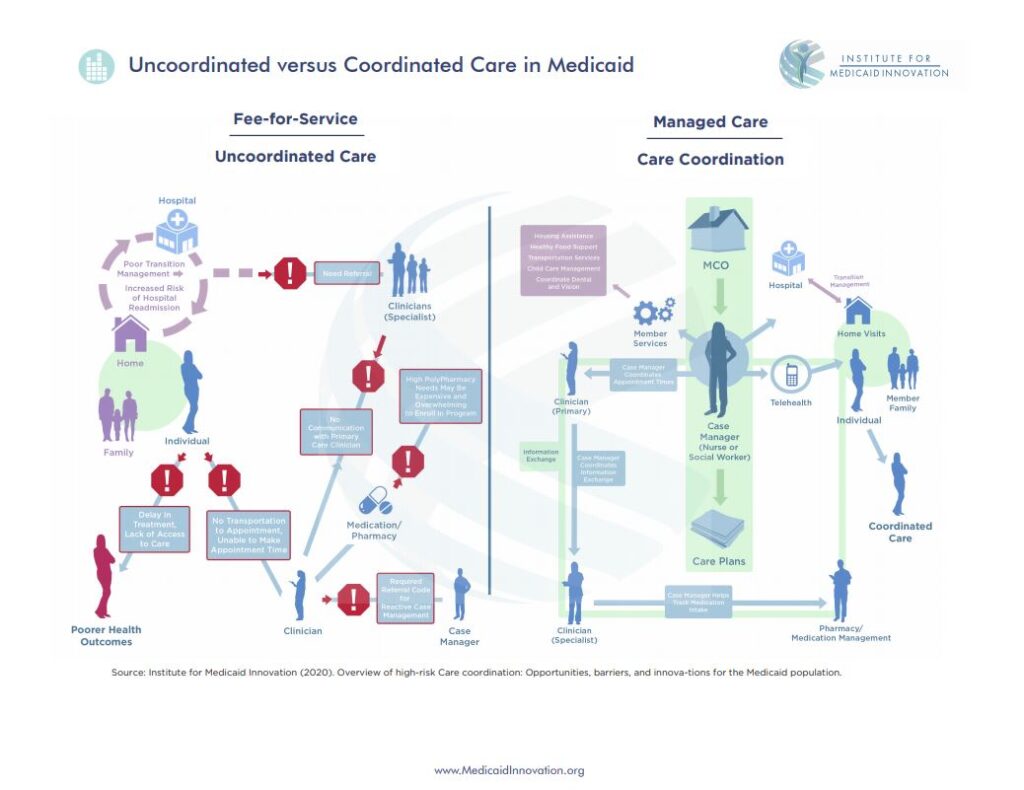
In a fee-for-service arrangement in Medicaid, care is not coordinated. The left side of the infographic depicts a typical care pathway for Medicaid enrollees who experience multiple chronic conditions and/or may have high rates of health care utilization. We begin with the individual, who encounters challenges in arriving for their primary care clinician appointment due to structural barriers such as transportation. Once the member completes their primary care appointment, there is limited communication or coordination with the specialist, which can lead to duplicative care. The lack of communication between clinicians about the member’s care plan can also lead to confusion for the member; for example, medication management may be difficult as members may be taking multiple medications that have different doses and schedules. For those receiving care from the hospital, without coordinated transition management from the hospital to outpatient care in the home setting, Medicaid enrollees may enter a cycle of hospital readmission. Of note, there are case managers on the “uncoordinated” side of the infographic; however, in fee-for-service Medicaid, clinicians must refer out care coordination services, often making the care management reactive rather than proactive.
In a managed care arrangement in Medicaid, a hallmark of the services and supports is care that is coordinated. The right side describes outlines how coordinated care benefits the member and creates a system of efficiency in the delivery of care. Medicaid managed care organizations assign case managers, typically nurses or social workers, to members based on their individual needs and goals. Collaborating with the enrollee and their families, the case managers create individualized care plans and provide an array of services that address many of the barriers depicted on the left side of the graphic, including coordinating information exchange between primary care clinicians and specialists, monitoring medication intake, and arranging housing assistance, food support, transportation services, and child care. Other care coordination services provided by case managers through Medicaid managed care organizations include transition management, telehealth, and home visiting services that can help reduce rates of hospital readmission, keep individuals engaged with their care plan, and continuously assess and respond to the enrollees’ needs.
The infographic provides a broad overview of the benefits and services associated with care coordination. For more information on HRCC, including clinical, research, and policy opportunities to improve the quality of and access to care coordination for the Medicaid population, access the full IMI report here.